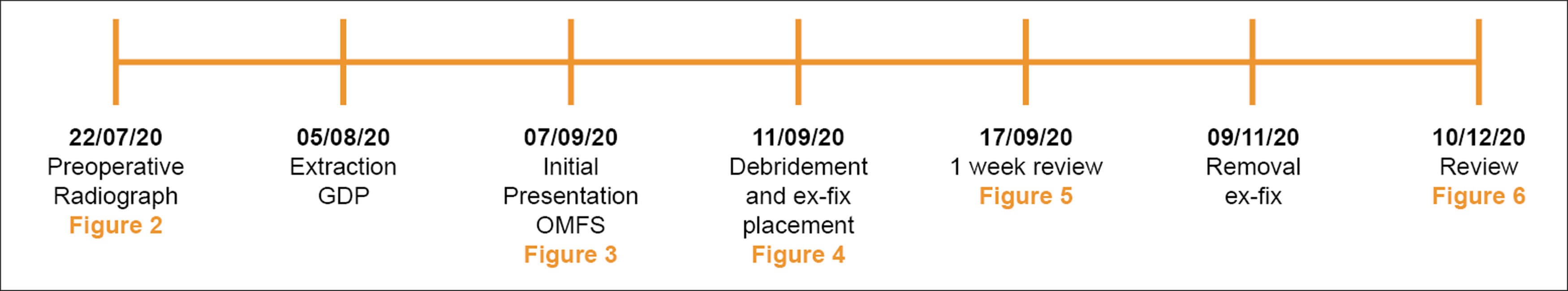
Figure 1: Timeline detailing key events in the patient’s treatment.
Whilst commonly affecting the feet, spine and hips in adults, osteomyelitis (OM) can also present to the oral and maxillofacial surgery (OMFS) clinic as pathology of the jaws. Case reports from Africa have described this condition as a result of acute necrotising ulcerative gingivitis or cancrum oris, however, it can also be found after a dental extraction, oral surgery or mandibular fracture. Signs and symptoms include pain, swelling, trismus, dysphagia, paraesthesia, leukocytosis and purulent discharge.
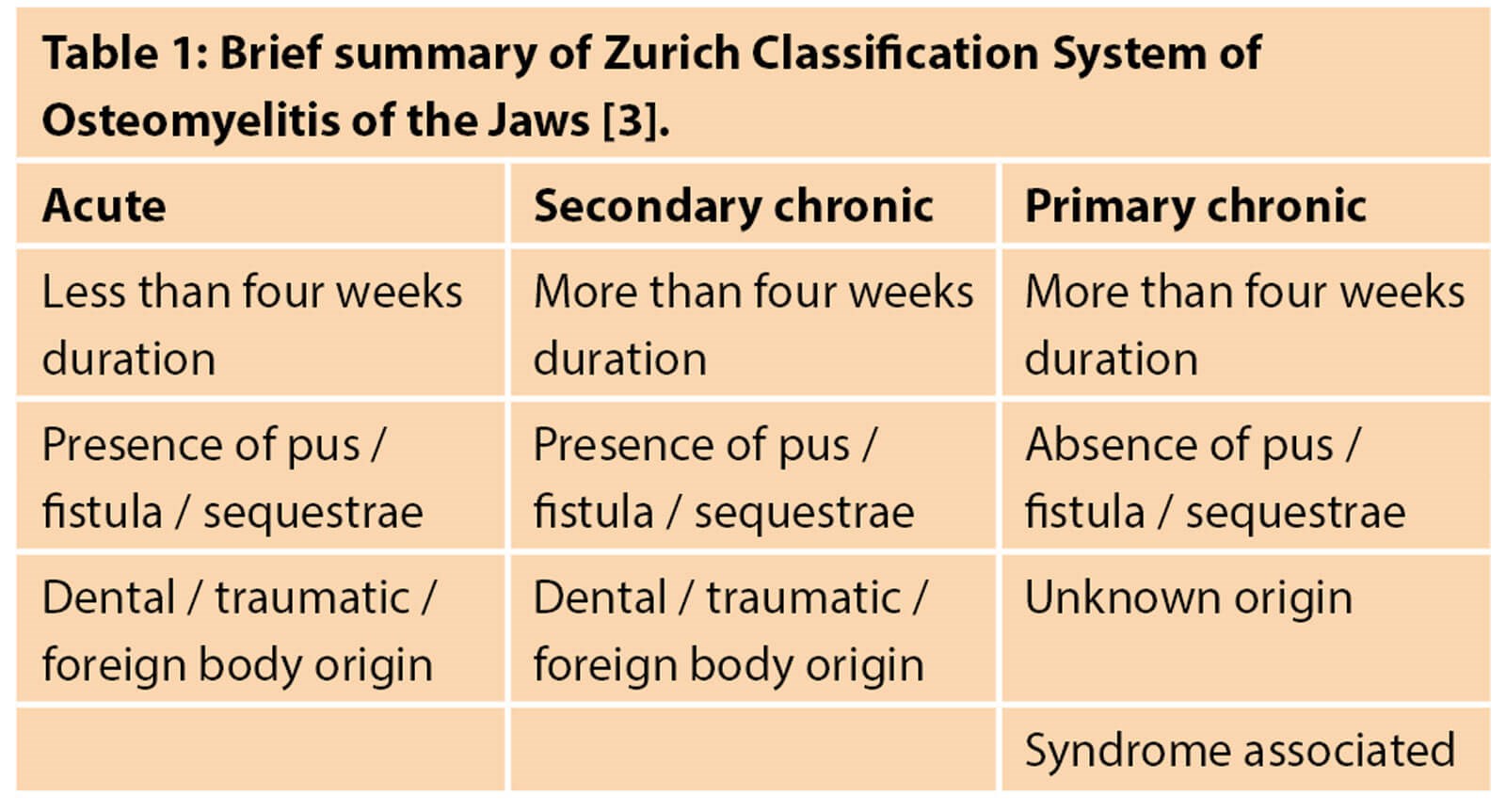
Microbiology results from OM of the jaws usually show an opportunistic, polymicrobial infection, caused primarily by a mixture of aerobic and anaerobic bacteria from the oral cavity [1]. This contrasts to OM of the long bones, usually caused by a Staphylococcus aureus infection [2]. Due to these differences in the pathogenesis, several different classification systems have been proposed specifically for the jaws. Of these, the Zurich classification appears the most widely used. In this, OM is categorised as acute, primary chronic or secondary chronic. The features of these are summarised in Table 1 [3].
Initial treatment is often empirical antibiotics, followed by targeted antibiotics after culture and sensitivity results – surgical debridement may be indicated in chronic cases that do not respond to antibiotic therapy [4].
Here, we present a case of a pathological mandibular fracture in a background of OM following a dental extraction in a type I diabetic, and its successful management with external fixation.
Case report
A 27-year-old female patient was referred by her general dental practitioner to our OMFS clinic presenting with trismus, malocclusion and paraesthesia of her right inferior alveolar nerve.

Figure 2: Preoperative radiograph of lower right first molar.
The patient had a lower right first molar extracted one month prior, due to a diagnosis of gross caries and acute apical abscess (Figure 2). They reported pain and swelling from this tooth for several years prior to visiting her general dental practitioner. Medically, she suffers from poorly controlled type-1 diabetes mellitus and takes regular insulin injections with an HbA1c on initial presentation of 91. Socially, the patient is married with two young children, does not drink alcohol but uses e-cigarettes regularly.
On examination, a palpable swelling to the right body of mandible in the lower right molar region was found, with no associated lymphadenopathy. Mandibular movements showed no dysfunction. The lower right first molar extraction site was swollen and tender, with protruding mobile hard tissue but no suppuration was seen. A premature contact was noted UR5, with an anterior and left-sided open bite. A patient-reported paresthesia of her right lower lip had been present since extraction.

Figure 3: OPG showing extent of osteomyelitis at presentation to OMFS department.
An Orthopantomagram (OPG) demonstrated a pathological fracture through extensive OM area around the right body of the mandible with proliferative periostitis indicating chronicity (Figure 3). A cone-beam CT scan confirmed this fracture.
A working diagnosis of a pathological right body mandibular fracture due to osteomyelitis following a dental extraction was made. This was then further subclassified as secondary chronic OM.
The provisional treatment plan was suggested as external fixation, debridement, biopsy of socket and micro samples. As the patient was unsure that she wanted to proceed with surgery, empirical amoxicillin was initially prescribed to treat the infection. The patient promptly indicated that she would like to go ahead with surgical management.

Figure 4: Photograph showing external fixator in place.
Four days after the initial presentation, the patient attended for external fixation of her mandible. The procedure involved raising a conservative mucoperiosteal flap lower right second molar to the lower right canine. The area of OM was thoroughly debrided and washed with saline 0.9% and hydrogen peroxide solutions. The lower border of the mandible was identified with a callus joining the segments with evidence of the mental nerve exiting its foramen. The fracture was manipulated and a functional occlusion established; 2x7mm and 2x11mm self tapping screws were placed and the external metal bar seated and tightened (Figure 4). Flap closure was achieved and 10ml of 0.5% chirocaine was given for postoperative analgesia. The UR6, UL6 and LL6 were also extracted at this time due to patient wishes, and glycaemic control was optimised on the ward. A fresh specimen was sent to microbiology for culture and sensitivity (C+S) testing, with a bone sample sent for histology. The C+S showed a general mixed picture of aerobic and anaerobic bacteria, with no particular predominant or pathogenic isolate. Histopathology demonstrated non-viable bone, fragments of inflamed granulation tissue, acute inflammatory cells and evidence of resorption with osteoclastic rimming – all features in keeping with the clinical history.
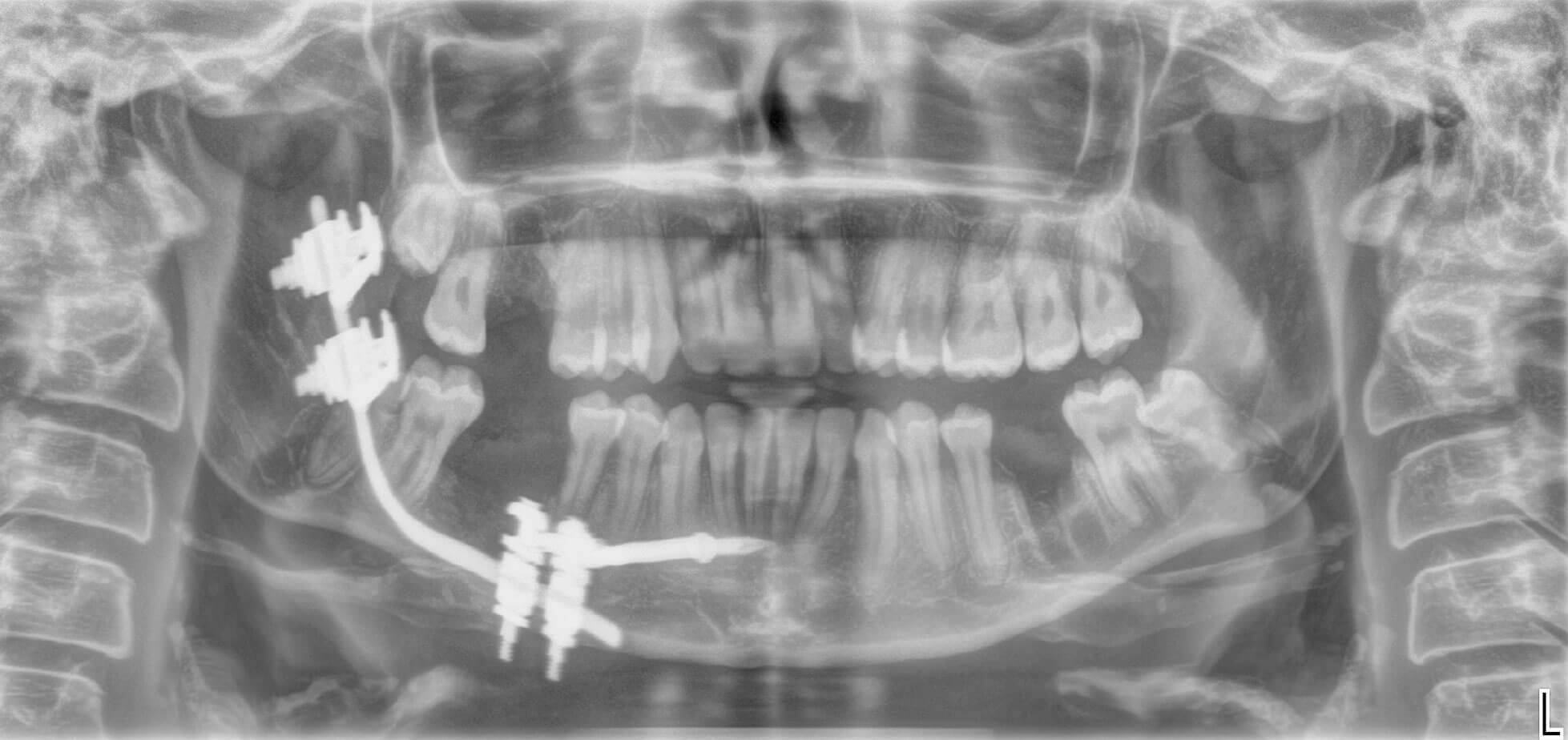
Figure 5: OPG showing external fixation in place.
The patient was then reviewed in one week’s time and an OPG was taken at this appointment (Figures 5). At this appointment, the patient reported minimal pain. On examination, the external fixation was stable, with evidence of intraoral healing.The patient was then reviewed four and six weeks post ex-fix placement. No issues were identified and good mucosal healing with no inflammation or infection was apparent. At the six-week review, the mucosa appeared well healed and the patient’s numbness had almost completely resolved. The OPG showed good bony infill.
The device was removed unremarkably under general anaesthetic eight weeks postoperative, with no mobility of the mandible evident immediately post removal.

Figure 6: OPG showing healing three month post ex-fix placement.
The patient was reviewed one month after device removal with no issues, and an even, stable occlusion. A postoperative radiograph confirmed good bony infill and no evidence of further infection (Figure 6). One final review at six months has been organised before formal discharge.
Discussion
This case demonstrates several interesting points for discussion. Whilst OM can be seen post dental extraction, it is not a regular occurrence. It is well known poorly controlled diabetic patients are more prone to infection, due to a compromise in both immune system and vascular supply, so it should not be surprising that this could extend to the jaws.
Whilst OM can be treated with antibiotics alone, other adjuvant therapies can be used to improve patient outcome, especially in chronic cases, such as surgery or hyperbaric oxygen therapy [4]. Unfortunately, in this case, the condition had led to a mandibular fracture, severely affecting occlusion, mouth opening and thus function and quality of life. Therefore, even if the chronic infection could be managed conservatively, surgical management is indicated to reduce the fracture and restore function. The usual technique for this would be the open reduction and internal fixation (ORIF) of a traumatically fractured mandible. However, the soft tissue envelope surrounding the fracture site was compromised in this case, preventing adequate internal plate coverage. Chronic OM is predominantly a biofilm infection, persisting on bony sequestrae and medical devices even after antibiotic use, increasing the risk of further chronic OM in open fractures treated with internal fixation [5]. In a case where a pathological biofilm is already established, placing an internal device would therefore increase risk of failure to cessate the infection and prevent adequate stabilisation, and so it was decided to use an external device.
It is important to fully manage a patient’s expectations in cases where external fixation is used to aid treatment compliance. If the patient is not fully aware of the implications a mandibular external fixator will have on their appearance short-term, then this could lead to a refusal to keep in place for the full duration of treatment, compromising effectiveness and a good clinical outcome. Therefore, it must be stressed preoperatively what the patient should expect, and to ensure that they are willing to wear an external fixator. As this case was carried out in the midst of the COVID-19 pandemic, face masks were worn almost everywhere away from home. The patient reported this was a great benefit, as she had an easy way of concealing the device and so felt much less self-conscious.
As certain conditions predispose to OM [6], should these patients be counselled in the increased risk of a bone infection prior to dental extractions? It is common practice to advise the risk of postoperative infection, but this case highlights the importance of describing to these patients how debilitating these infections could be. There is no current system for stratifying patients into risk categories for OM post dental extraction. However, as OM is a recognised complication of extraction, being able to categorise patients into high and low risk groups would better inform patients to consent for a procedure.
Conclusion
External fixation devices are not currently routinely used and may have negative connotations from a patient’s perspective due to their appearance; however, in cases with an established pathological biofilm with a compromised soft tissue envelope, they can be a useful addition to the oral and maxillofacial surgeon’s armamentarium, giving a good postoperative outcome in the management of pathological fractures of the mandible.
References
1. Gaetti-Jardim Júnior E, Fardin AC, Gaetti-Jardim EC, et al. Microbiota associated with chronic osteomyelitis of the jaws. Braz J Microbiol 2010;41(4):1056-64.
2. García Del Pozo E, Collazos J, Cartón JA, et al. Bacterial osteomyelitis: microbiological, clinical, therapeutic, and evolutive characteristics of 344 episodes. Rev Esp Quimioter 2018;31(3):217-25.
3. Baltensperger M, Grätz K, Bruder E, et al. Is primary chronic osteomyelitis a uniform disease? Proposal of a classification based on a retrospective analysis of patients treated in the past 30 years. J Craniomaxillofac Surg 2004;32(1):43-50.
4. Lima AL, Oliveira PR, Carvalho VC, et al; Diretrizes Panamericanas para el Tratamiento de las Osteomielitis e Infecciones de Tejidos Blandos Group. Recommendations for the treatment of osteomyelitis. Braz J Infect Dis 2014;18(5):526-34.
5. Zimmerli W, Sendi P. Orthopaedic biofilm infections. APMIS 2017;125(4):353-64.
6. Roy M, Somerson JS, Kerr KG, Conroy JL. Pathophysiology and Pathogenesis of Osteomyelitis. InTech Open 2012 10.5772/32171.
Declaration of competing interests: None declared.
COMMENTS ARE WELCOME







