
The repair of postoperative perineal hernias is extremely challenging. Two male patients with problematic secondary perineal hernias following abdominoperineal resection of rectal adenocarcinoma have been successfully treated using the Ventralex™ composite, self-expanding ventral patch, normally used for umbilical and epigastric hernia repairs. The rationale for the use of and the technique of effective placement of the patch will be discussed.
Case report
A 63-year-old male, with a history of insulin-dependent type 1 diabetes mellitus, underwent successful treatment of a rectal adenocarcinoma with chemoradiotherapy and laparoscopic extra-levator abdominoperineal resection. However, six months later whilst straining at work, he developed an enlarging, painful, perineal swelling. On clinical examination, the perineal swelling measured 10cm by 6cm and was easily reducible (Figure 1). Upon investigation, a CT scan revealed loops of small bowel in the hernial sac and no other abnormality.

Figure 1: The patient standing, preoperatively, with the perineal hernia evident.
Preoperatively, at a combined colorectal / plastic surgery clinic, a decision was made to utilise a self-expanding, flexible, composite polytetrafluoroethylene (PTFE) / polypropylene mesh to reinforce the operative repair. The rationale was that with the patient in the erect or supine position, the intra-abdominal contents would lie on the internal surface of the composite mesh, allowing the flange of the device to abut the edges of the hernial defect, thus potentially reinforcing and strengthening the repair.
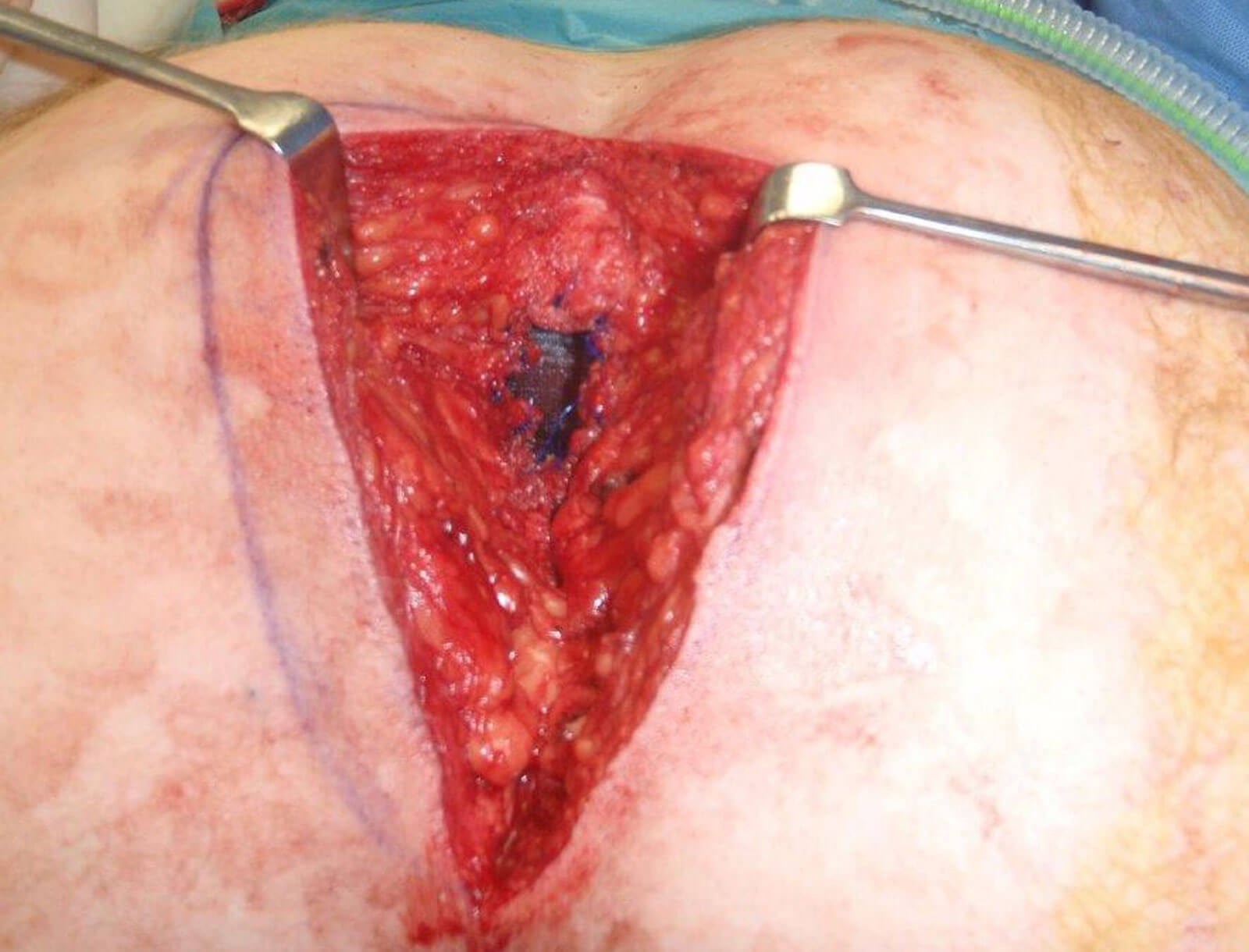
Figure 2: The Ventralex™ composite mesh in place in the patient’s hernial opening.

Figure 3: The completed repair.
In theatre, under general anaesthesia with the patient in the prone position, the hernial sac and thinned redundant skin were excised and the small bowel was dissected free from the hernial opening, providing a ledge for the mesh to lie on. An 8cm sterile Ventralex™ self-expanding, flexible composite PTFE / polypropylene laminate mesh was easily placed and positioned with the flange abutting the internal edges of the defect, deep to the hernial defect, with the straps facilitating its intra-peritoneal placement. Fixation sutures of 2/0 prolene were used to attach the polypropylene portion of the mesh to the hernial edges and the surrounding fascial tissues were then re-approximated to further reinforce the repair (Figure 2). The adjacent skin and subcutaneous tissues were then undermined, advanced and closed in layers (Figure 3) and a suction drain left in-situ for 24 hours.

Figure 4: The perineal wound site, 12 months postoperative.
The perineal problem was successfully resolved, with no subsequent symptoms or recurrence of the hernia, 24 months on from surgery (Figure 4). This simple method of perineal reconstruction was also successfully used on another patient with a similar presentation who had undergone an open index operation, as opposed to a laparoscopic procedure, as in the previous patient. Both patients remain well with no recurrence of either hernia at 24 months following successful surgical repair.
Discussion
A secondary perineal hernia is a rare yet challenging complication following abdominoperineal surgery and refers to the protrusion of intra-abdominal viscera through the pelvic floor defect [1] following, in this case, resection of the patient’s rectal adenocarcinoma. The incidence of perineal hernia following abdominoperineal and extralevator abdominoperineal excision is between 1 and 26%, occurring most commonly within the first postoperative year [1]. Contributing risk factors for postoperative perineal hernia have been found to include preoperative radiotherapy, smoking, omentoplasty, and postoperative perineal wound infection [2].
In our patients, the primary surgical procedure was an abdominoperineal resection of a rectal carcinoma, which is an ablative and destructive procedure, potentially resulting in large perineal defects which can be primarily closed directly or by the use of synthetic or autologous tissue [1,2]. Delayed healing of the perineal wound is a potential postoperative complication, alongside wound dehiscence, local infection, pelvic abscess formation and enteric fistulae. The risk of an occurrence of a postoperative wound complication is greatly increased by neoadjuvant chemo-radiotherapy [1,3,4].
In the first patient, who had undergone laparoscopic abdominoperineal resection, there were minimal pelvic and perineal adhesions. The second patient, who had undergone open abdominoperineal resection, had small bowel which was densely adherent to the pelvic sidewall and perineal defect. Adhesions in these patients should therefore be anticipated and planned for with meticulous dissection performed. Small bowel injury, mesh infection and / or fistulation would be disastrous in these patients, and all possible preventative measures should be employed.
A postoperative perineal hernia repair is extremely demanding with a potentially high rate of recurrence [2]. The procedure can be performed using the perineal approach, laparoscopic approach, open abdominal approach, laparoscopic perineal approach or the open abdominoperineal approach [1]. The technique may involve the use of a non-absorbable mesh, composite and biological mesh or by the addition of myo-cutaneous flaps, such as Gracilis muscle and rectus abdominus to augment the repair [1], with another option being the inferior gluteal artery flap.
In these particular cases, a decision was made to employ the Ventralex™ self-expanding composite PTFE / polypropylene mesh to reinforce the hernial repair. This patch can be easily placed behind the hernial defect through a perineal incision, avoiding the addition of laparoscopy or a laparotomy [5]. The rationale behind its application was that the outer flange of the device would be contiguous and lie on the internal edge of the intra-abdominal surface of the hernial defect, thus strengthening the repair as the bowel would mold the two surfaces together.
Twenty-four months following successful perineal hernia surgical repair, there has been no sign of recurrence of the condition in either patient. Both procedures were carried out on the same day and the patients discharged the following morning.
Conclusion
Surgical restoration of two postoperative perineal hernias has been successfully performed with a composite laminate mesh, normally used in the repair of ventral hernias. By abutting the flange of the patch behind the defect on the inner peritoneal aspect of the hernial opening, a more robust form of permanent repair is possible. We would recommend it for consideration in the repair of these most challenging of cases.
TAKE HOME MESSAGE
-
Combined working is in the patient's best interests
-
Preoperative planning is crucial
-
Frequently, simpler forms of reconstruction are very effective
-
Be prepared to think outside of the box
References
1. Balla A, Batista Rodríguez G, Buonomo N, et al. Perineal hernia repair after abdominoperineal excision or extralevator abdominoperineal excision: a systematic review of the literature. Tech Coloproctol 2017;21(5):329-36.
2. Blok RD, Brouwer TPA, Sharabiany S, et al. Further insights into the treatment of perineal hernia based on a the experience of a single tertiary centre. Colorectal Dis 2020;22(6):694-702.
3. Artioukh DY, Smith RA, Gokul K. Risk factors for impaired healing of the perineal wound after abdominoperineal resection of rectum for carcinoma. Colorectal Dis 2007;9(4):362-7.
4. Bullard KM, Trudel JL, Baxter NN, Rothenberger DA. Primary perineal wound closure after preoperative radiotherapy and abdominoperineal resection has a high incidence of wound failure. Dis Colon Rectum 2005;48(3):438-43.
5. Martin DF, Williams RF, Mulrooney T, Voeller GR. Ventralex mesh in umbilical/epigastric hernia repairs: clinical outcomes and complications. Hernia 2008;12(4):379-83.
Declaration of competing interests: None declared.
Informed consent:
Informed consent was obtained from the patient regarding the photographs used, and the publication of this article.
Acknowledgement:
All images belong to Mr Neil R McLean.
COMMENTS ARE WELCOME








