As the demand for natural results in aesthetic medicine increases, both patients and physicians are more educated in the complex ageing process of the face. Instead of chasing lines, a more global facial approach with strategic placement of deep volume, is ideally chosen for facial rejuvenation. And even though the ageing process differs from person to person, it also is predictable. And that’s why a general protocol can be described for my personal approach to treating the whole face with soft tissue fillers [1].
The frontal concavity is believed to be the result of mainly bone remodeling [2,3]. Ideally, a thick filler should be placed in the subgaleal space to allow for natural results on lifting of the brows. To avoid intra-arterial injection and potential blindness, non-traumatic cannulas should be used in this area with entry holes at the medial border of the temporal crest and potentially the midline.
The temporal area ages due to bone resorption, lipoatrophy and muscular atrophy [4]. The volumising filler can be placed on the periosteum using either needle or cannula. When using needles, care should be taken not to inject with high pressure or with high volumes with a static needle tip, to avoid complications associated with intravascular injection. It is safer to use cannulas: at the lateral border of the temporal crest an entry point can be located 1-2cm cranial to the orbital rim from where an opening can be made in the deep temporal fascia through which the cannula can be manoeuvered and advanced over the periosteum.
The cheeks age due to bone resorption of the maxilla, the zygoma and of deep fat [5,6]. Apart from volume loss, skin laxity contributes to the descent of the cheek because of reduced capacity to fixate the soft tissue on its anatomical position.
Augmetation should therefore target both deep volume and superficial neocollagenesis. Using non-traumatic cannulas, a two-point technique can be used where the first entry point can be found on the zygomatic arc, just in front of the hairline. From this point, the cannula should be manoeuvered through the superficial muscular aponeurotic system (SMAS) to the preperiosteal fat, where the full thickness soft-tissue filler can be placed; either in retrograde strands or in multiple boluses. Caudally from the bone, a product should be chosen that simulates neocolagenesis.
At the lower border of the zygoma, just lateral to the nasojugal groove, a second entry point can be found. The full-thickness filler should be placed in the preperiosteal fat, in the deep medial fat compartment, or in the Ristow space. The cannula can be advanced all the way up to the orbicularis retaining ligament, which is the most cranial border of the treatment zone. Inferior to the zygoma, neocollagenesis should be stimulated in the skin.
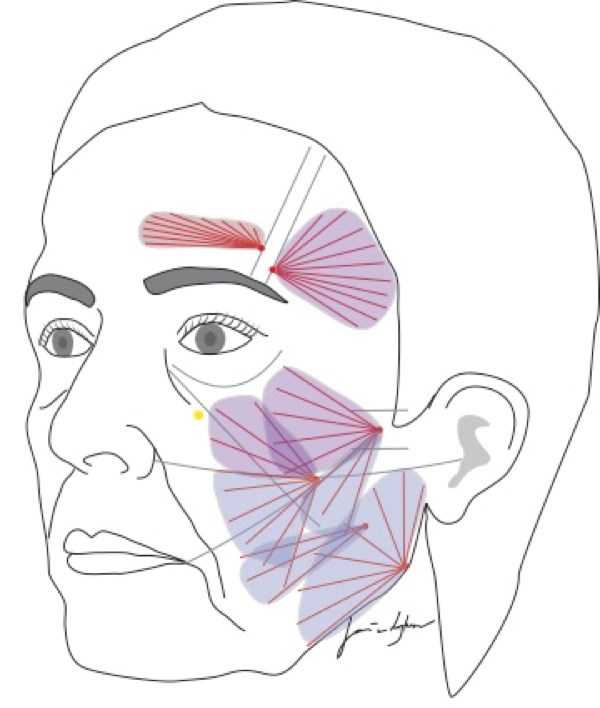
Figure 1: Schematic drawing of the basic treatment protocol. Frontal concavity: medium to thick hyaluronic acid in the subgaleal space. Temporal area: volumising soft-tissue filler supraperiosteally and, if required, hyperdiluted calcium hydroxylapatite subcutaneously (1.5ml of product is mixed with 0.6 to 1.0ml of lidocaine; this off-label mixing allows for easy even distribution of product, as the original product has a very high viscosity and injection can lead to visible product strands). Cheeks: Multilevel technique: volumising soft-tissue filler supraperiosteally and hyperdiluted calcium hydroxylapatite subcutaneously. Deep injection above the marked alar-trachal line and superficial injection under this line. Mandibular angle: Multilevel technique: volumising soft-tissue filler supraperiosteally (under masseter) and hyperdiluted calcium hydroxylapatite subcutaneously, with extra thick strands at the edge of the lower margin of the mandible to accentuate the definition of the jawline.

Figure 2: Left: before treatment. Right: after 6ml calcium
hydroxylapatite and 1ml medium thickness hyaluronic acid.

Figure 3: Left: before treatment. Right: after 7.5ml calcium hydroxylapatite.
Ageing of the mandible is characterised by dorsal and caudal bone resorption, resulting in widening of the mandibular angle [7]. Dermal ageing is characterised by collagen reduction. The mandibular angle can be treated by dermal stimulation of neocollagenesis alone, or combined with submuscular volumisation with a volumising filler, although the bigonal distance of the mandibular angles does not change during the aging process. Ageing of the lower cheek is characterised by volume loss and dermal laxity. Care should be taken to avoid injecting product in the jowls, as this could aggravate the aged appearance. Figure 1 shows products and injection patterns of choice.
References
1. Van Loghem J, Yutskovskaya Y, Werschler P. Calcium hydroxylapatite over a decade of clinical experience. J Clin Aesthet Dermatol 2014;7:38-49.
2. Richard MJ, Morris C, Deen BF, et al. Analysis of the anatomic changes of the aging facial skeleton using computer-assisted tomography. Ophthal Plast Reconstr Surg 2009;25:382-6.
3. Pessa JE. An algorithm of facial aging: verification of lambros’s theory by three-dimensional stereolithography, with reference to the pathogenesis of midfacial aging, scleral show, and the lateral suborbital trough deformity. Plast Reconstr Surg 2000;106(2):479-88.
4. Binder WJ. Facial rejuvenation and volumisation using implants. Facial Plastic Surgery 2011;27:86-97.
5. Mendelson B, Wong CH. Changes in the facial skeleton with aging: implications and clinical applications in facial rejuvenation. Aesthetic Plast Surg 2012;36(4):753-60.
6. Warren RJ, Aston SJ, Mendelson BC. Face lift. Plast Reconstr Surg 2011;128:747e-764e.
7. Shaw RBJ, Katzel EB, Koltz PF, et al. Aging of the facial skeleton: aesthetic implications and rejuvenation strategies. Plast Reconstr Surg 2011;127:374-83.
COMMENTS ARE WELCOME




