In this second part of this two-part article we begin by looking at component separation which is a technique of reconfiguring anatomical layers to allow intrinsic reconstruction of the integrity of the anterior abdominal wall. We then move into the domain of flaps but these are not typical flaps. By definition a flap comprises reconstructive tissue that retains its vascularity during positional transfer. Flaps can be categorised and defined in a number of ways including composition, vascular supply and movement.
Component separation
Component separation was brought to the forefront in 1990 by Ramirez et al. as another option for midline abdominal wall reconstruction [1]. This is an increasing problem in the era of obesity, burst abdomens and ventral hernias. Component separation restores the integrity of the abdominal wall and variations of the technique are present in the literature as early as 1916 (Gibson et al.). The technique involves a bipedicled advancement flap involving the rectus abdominis muscles, internal oblique and transversus abdominis muscles with or without a supplemental mesh. It remains a neurotised flap and can allow functionality that can provide stable soft tissue coverage with a good cosmetic appearance.
It is most commonly indicated in repair of large, midline abdominal wall incisional hernias that have failed suture closure or mesh repair or secondary to abdominal wall resection due to malignancy or trauma. The type of defect that can be repaired is in the midline and up to about 20cm in diameter. It is also important to identify previous incisions and whether they may have compromised the innervation or blood supply of the abdominal components. In particular the superior and deep inferior epigastric arteries, which supply the rectus flap in conjunction with segmental intercostal vessels, if disrupted the rectus is supplied by collaterals from the internal oblique and the transversus abdominis muscles.
The component separation method disconnects the muscle layers from their fascial sheaths to allow separate expansion of each muscle and a larger surface area. In the anterior approach, the abdominal pannus is carefully elevated from the underlying rectus and external oblique fascia, an incision is made in the external oblique aponeurosis 2cm lateral to the border of the rectus and external oblique muscles (i.e. semilunar line) and extending from the costal margin to the inguinal ligament.
Separation of the external oblique muscle from the underlying internal oblique muscle results in approximately 5cm of advancement in the upper third of the abdomen, 10cm in the mid abdomen, and 3cm in the lower third of the abdomen. If this is not sufficient, the rectus muscle can be dissected free of its posterior sheath. This can lead to an additional 2 to 4cm of flap advancement. Some modification includes the use of mesh to reinforce the repair or an endoscopic method which can minimise ischaemia to the skin flaps.
Recurrence rates for component separation repair without mesh are not significantly different from standard mesh hernia repairs but rates using mesh appear to be slightly lower, ranging from 4-10%.
“It led to an understanding that in highly selected cases significant improvement can be achieved in providing dignity and an improved quality of life in the dying patient.”
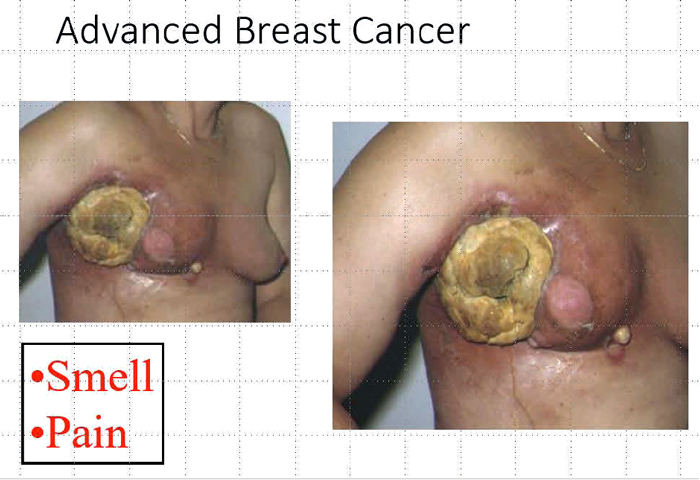
Figure 1.
Flaps
The local fillet flap:
Figure 1 demonstrates the case of Susan, an incredibly brave woman, dying from advanced breast cancer, has been shared before in an open access editorial written in JPRAS [2]. This was a desperate measure to improve the quality of life of a dying patient and perhaps it was luck that it had such a dramatic and positive effect. But it led to an understanding that in highly selected cases significant improvement can be achieved in providing dignity and an improved quality of life in the dying patient. It is beyond the scope of this present article to discuss the philosophy and ethics of surgical palliation but it must be a consideration. Some years later when submitting a series of cases for publication in internationally recognised palliative care journals the response of the reviewers was uniformly prejudiced and biased. The palliative care physicians could manage pain, they could manage smell, they could manage the psychological distress of patients and there was no place for surgery. After repeated rejections in palliative care journals we submitted our paper to surgical journals. The response was initially bizarre; this was not evidence-based, we did not have randomised controls, etc. Finally, we found a journal with pragmatic editors who recognized the unique nature of our work and a case series was published [3].
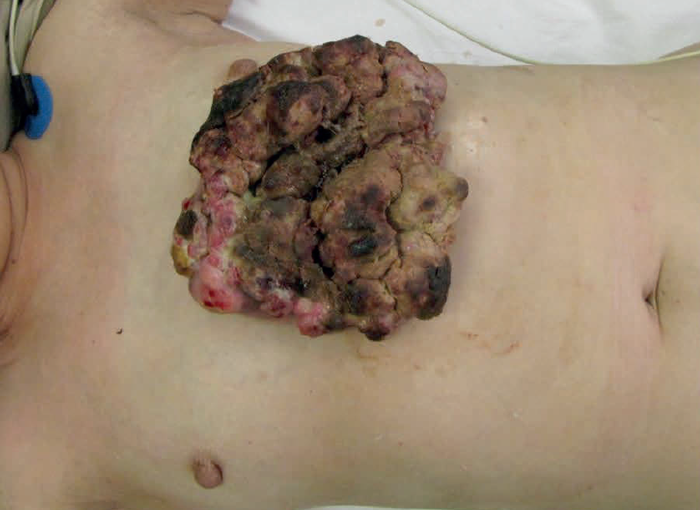


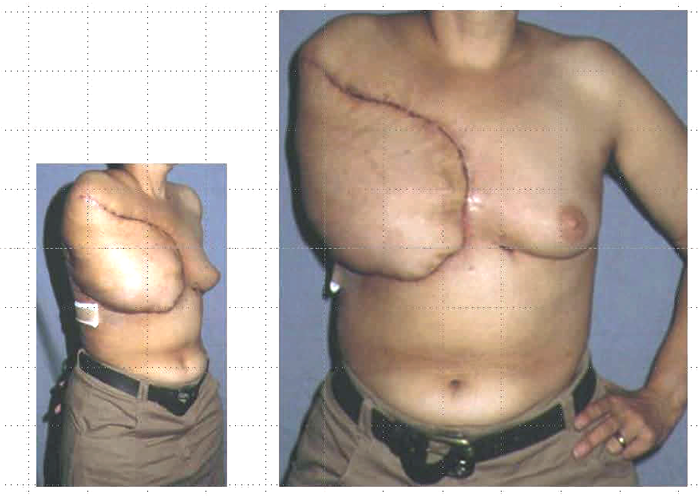
Figure 2.
A local transposition flap:
The principle of transposing local tissue to reconstruct a defect created following tumour excision is well established. It is simple geometry and the principles can be scaled up. In Figure 2, a 56-year-old female patient presented with a two-year history of a fungating chest wall tumour. MRI depicted a left anterior chest mass invading dermal and subcutaneous tissues and PET-CT confirmed multiple right lung nodules with increased uptake in the right axillary nodes. An incisional biopsy revealed a malignant spindle cell neoplasm although the origin, skin or breast, was in doubt. The tumour needed excision with a wide margin for quality of life reasons. Prior to excision the tumour was isolated in a betadine soaked gauze and a defect created. The ‘educated scalpel’ indicated involvement of the lower part of the sternum which was also excised. How then to reconstruct the defect? A simple transposition flap. At the same time a right axillary block dissection was performed.
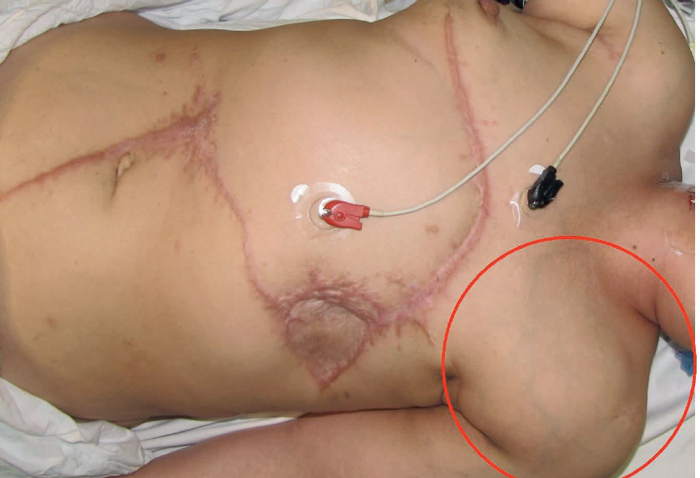
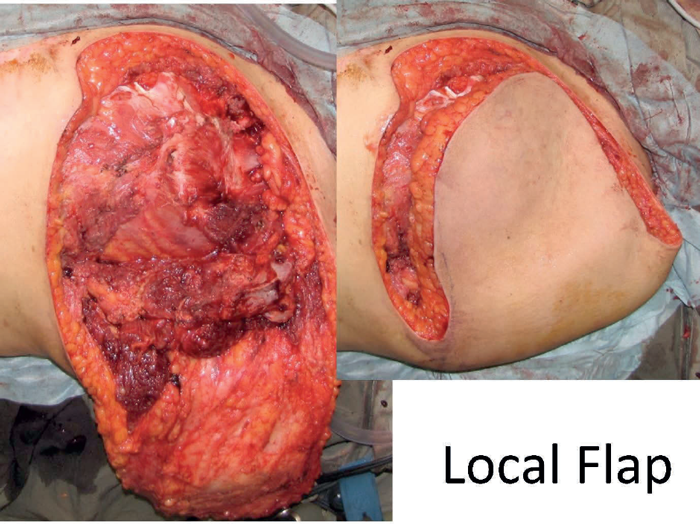

Figure 3.
Ten months later the patient re-presented with a large left supraclavicular mass (Figure 3). A forequarter amputation was performed with in continuity excision of the local recurrent tumour. The defect was closed with a simple local flap. Follow-up two years later reported the patient had returned to work, as a caretaker in an apartment block and there was no evidence of recurrent disease.
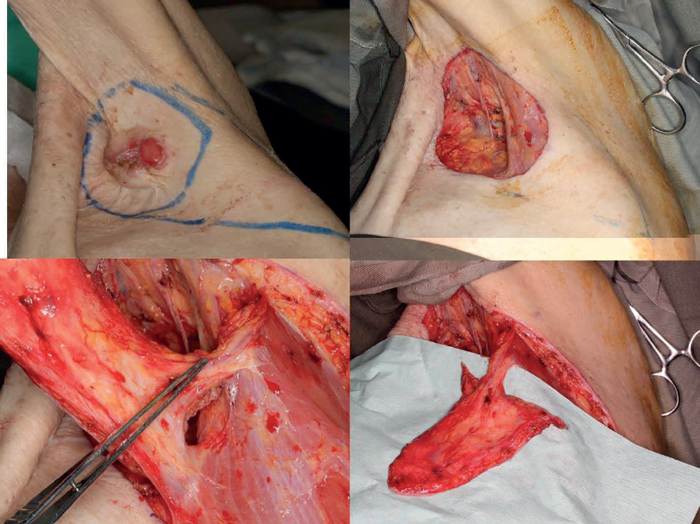
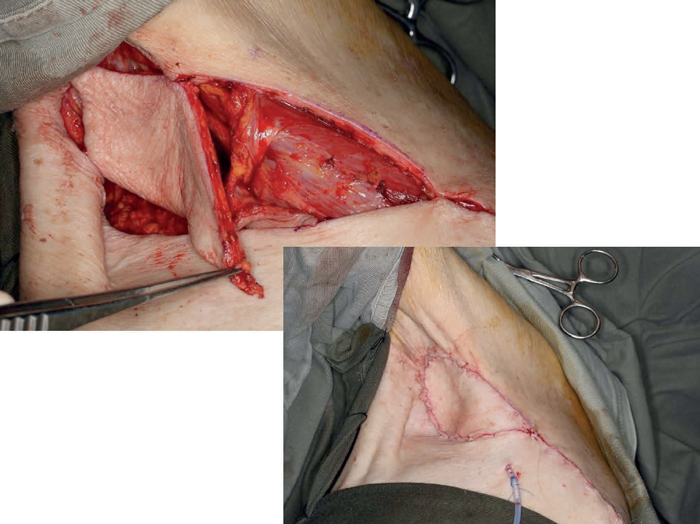
Figure 4.
Pedicled flaps:
When discussing the definition of a pedicled flap there is often some confusion regarding the composition of the pedicle and the anatomical relationship between the donor and recipient site. The first case (Figure 4) shows a simple V-Y advancement flap in the axilla based on a thoracodorsal artery perforator flap. This is not a complex wound but the case is included to illustrate a point although this may be contentious! The second case (Figure 5) shows a challenging fungating leiomyosarcoma on the right anterior chest wall. After excision, the defect could be closed with a pedicled latissimus dorsi flap, or a pedicled vertical rectus abdominis myocutaneous (VRAM) or transverse rectus abdominis myocutaneous (TRAM).

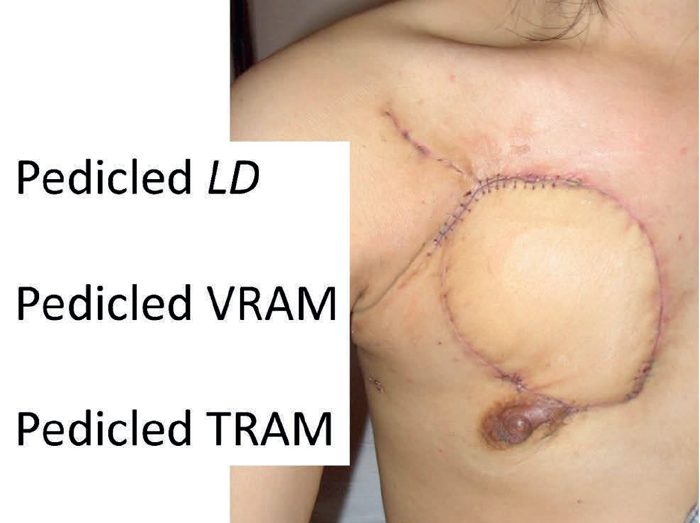
Figure 5.
Large abdominal wall defects can be closed with a pedicled anterolateral thigh flap as illustrated in the next case (Figure 6). The patient had a local recurrence after a previous hindquarter amputation. Faecal diversion had already been performed and now urinary diversion was needed before closure of the abdominal wall defect with a pedicled anterolateral thigh flap. The donor site was reduced in size by inverting the skin margins and the muscle was grafted. This is an example of quality of life surgery where not only the patient but also the relatives have to be considered. This patient, as was also the case with Susan (mentioned previously), had a devoted partner who struggled to support her whilst being overcome with nausea at the smell of the fungating tumour. Smell is a very powerful force with a strong subjective overlay and must never be discounted by professional health workers.
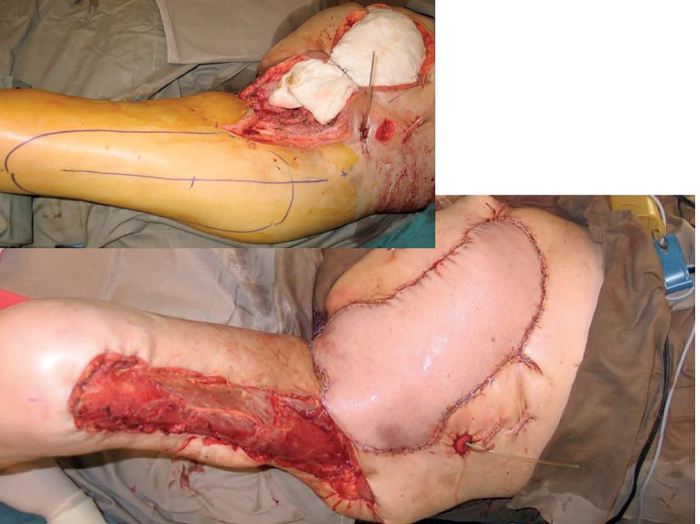
Figure 6.
Replacement of the entire abdominal wall can be achieved by a pedicled anterior thigh flap based on perforators from the combined vascular pedicles of the superficial femoral artery and the descending branch of the lateral femoral circumflex artery. In Figure 7 the abdominal wall had been previously excised and a mesh applied following tumour excision. A large flap can be used to cover from the pubis to the xiphisternum and the donor defect closed with t-split thickness skin graft.
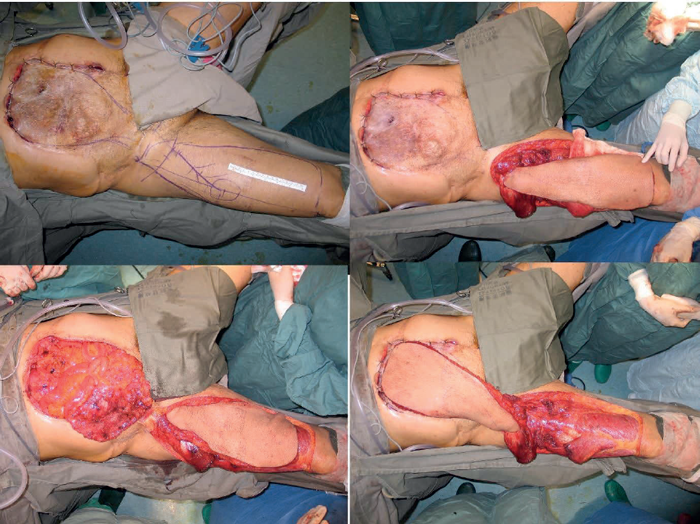

Figure 7.
Free tissue transfer:
Breast reconstruction using free tissue transfer is one of the more common operations performed in plastic surgery units in the UK. In Figure 8, the pathology was rather different being an angiosarcoma of the male breast. This case illustrates an interesting reflection of the difference between the healthcare systems in the UK and in Hong Kong. In the UK such a patient would typically go to their family doctor who would make a referral to an NHS centre where there would be a multidisciplinary team (MDT) who would discuss the most appropriate treatment. In Hong Kong there is not a well-established primary care service and if a patient does not go through the public service they would seek advice from a specialist de novo. Of course, the whole point of the MDT is to allow the respective specialists to discuss the merits and drawbacks of the various therapeutic strategies. Angiosarcoma is a challenging pathology which is usually radio-resistant. The patient realised that they most probably had a tumour and so decided to see an oncologist.
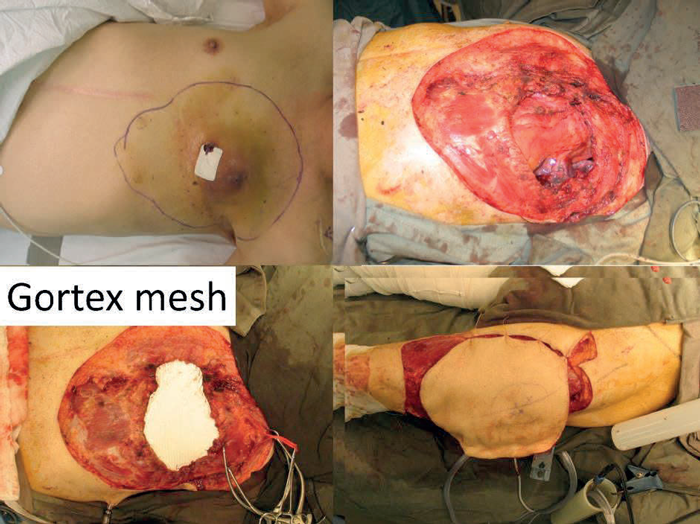
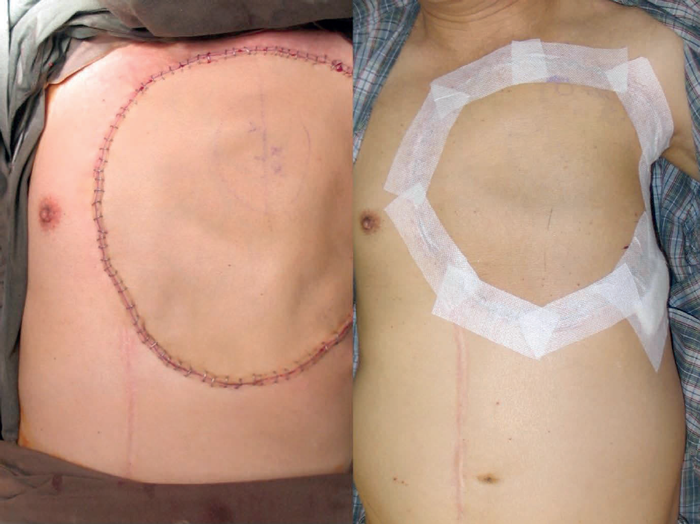
Figure 8.
The oncologist ordered imaging that revealed multiple pulmonary nodules and so used this to justify chemotherapy. After three cycles of chemotherapy there was a reduction in pulmonary deposits but the primary tumour remained unchanged and so at this stage referred the patient for a surgical opinion. The thought was that if the tumour mass could be debulked the residual malignancy might respond to the chemotherapy. The tumour was excised widely and in depth to leave a defect with exposed mediastinum and lung. The compartmentalisation of the thoracic cavity was reconstituted with a Gortex mesh. The skin defect was reconstructed with a large anterolateral thigh free flap and the patient was discharged home 10 days post-surgery.
Free fillet flap:
Fungating girdle tumour present both challenges in control but also opportunities in reconstruction. It is essential to be able to achieve proximal vascular control before attempting to ablate local disease. There is a fine line between surgical futility and surgical palliation. The situation is rather different from medical futility where the concept is to protect doctors from patients or relatives who will not accept that further treatment will result in no benefit. Laws were needed to protect doctors from being sued by patients or relatives when they refused to continue what was regarded as a futile treatment. The situation is different for surgery where patients have to be protected from surgeons whose belief in their surgical skills exceeds their practical abilities. Nevertheless, there will be cases where appropriate imaging can indicate the possibility of achieving vascular control enabling the resection of extremely large tumours. The point with girdle tumours is the distal limb may not be involved with any pathology and thus can be a source for reconstructive tissue which will not be associated with any donor site morbidity.

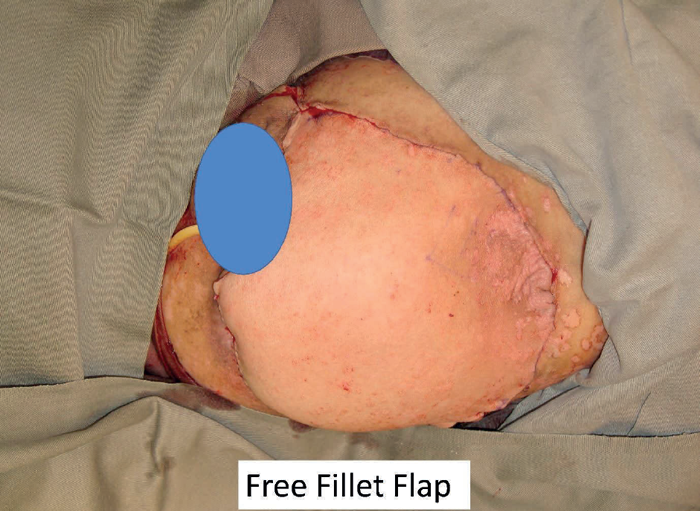
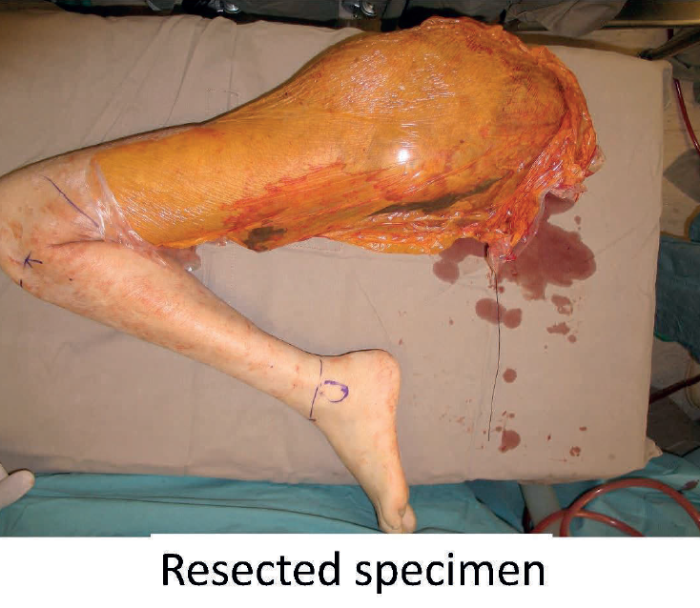



Figure 9.
The next patient (Figure 9) was a dramatic case of a massive fungating and bleeding tumour. After extensive discussion the patient consented to surgery. The resected specimen is shown which shows the lack of involvement of the distal lower leg. The soft tissues were stripped at periosteal level to allow a large flap to be raised to close the pelvic defect. The patient survived for 36 months and became a patient counsellor for other patients with advanced malignant disease. She gave full permission for her photograph to be used so that she could be an inspiration to others both in life and in death.
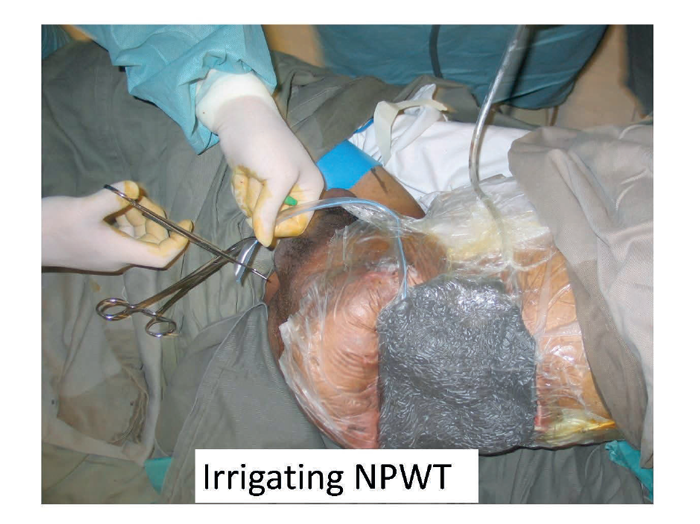
Negative pressure therapy:
No discussion of the management of complex wounds of the trunk would be complete without including the mention of negative pressure therapy. This has multiple roles including the active preparation of wounds for definitive surgical closure, closure without surgery and also in the comfort care of the dying patient. In this illustrated case (Figure 10) a young patient is shown who has had a hind quarter amputation and now progressive local disease has resulted in multiple faecal fistulas. Management of the wound was requiring painful dressing changes three times a day that was distressing for both the patient and the mother who insisted on caring for her dying son. The patient was taken to theatre for one final debridement and closure of the fistulas and the application of an irrigating negative pressure wound therapy device. No further dressing changes were necessary in the subsequent few days and the patient was allowed to die both in comfort and with dignity.
Figure 10.
Summary
This two-part article has covered a broad scope of reconstructive options which reflect a variety of technical challenges in the surgical procedures. It must be remembered though that it is the outcome as experienced by the patient and their relatives that is most important. The temporal element is very important when considering the implications of growth in children and value of days and weeks in the dying. In all cases we must be humble and honest in approach, yet brave and fearless, although not foolhardy, in execution.
References
1. Ramirez OM, Ruas E, Dellon AL. “Components separation” method for closure of abdominal-wall defects: an anatomic and clinical study. Plastic and Reconstructive Surgery 1990;86(3):519-26.
2. Burd A. Obituaries, death and dying. Journal of Plastic, Reconstructive & Aesthetic Surgery 2008;61(9):1003-4. 3. Burd A, Wong KC, Kumta SM. Aggressive surgical palliation for advanced girdle tumours. Indian Journal of Plastic Surgery 2012;45(1):16.
Declaration of competing interests: None declared.
COMMENTS ARE WELCOME