
Facial veins can be treated with a wide range of aesthetic and surgical procedures. Victoria Smith and Professor Mark Whiteley, both experts in the area, provide a comprehensive overview of diagnosis and the different treatment options available.
Patients with unwanted facial veins commonly present to aesthetic medicine practitioners. Problem veins on the face range from very superficial ‘capillaries’ to large bulging subdermal veins. In our practice we have found that, to provide a full service to these patients, we need a combination of traditional aesthetic approaches with a more invasive surgical approach. In addition, it is also important to be able to recognise facial veins that might be a sign of a more complex problem that should be referred away from an aesthetic practice.
Because of the combination of aesthetic or surgical treatments that might be needed, some patients are offered a joint consultation between aesthetic practitioner and venous surgeon. However, we have found that a few simple screening questions asked at the time of first enquiry, often backed up with a picture sent by the potential patient by email, can usually determine which one might be optimal to give the first opinion.
We classify facial veins in terms of how big and how deep they are, and where they are found – i.e. the size of the vein, the depth of vein – either within or under the dermis, and the anatomical area of the face affected. Fortunately, there is a good correlation between the anatomical location and what sort of vein is found in each location. Therefore, when we describe veins by the anatomical area on the face, it usually indicates what sort of vein is likely to be found.
Basic classifications of facial veins – size and depth of vein
Before going into the different classification of each sort of vein, it is important to remember that the venous system is a network of little veins, draining into larger veins. It is often called ‘branching’ although in reality, it is the reverse of branching. Thousands of little veins (called venules) drain venous blood from capillaries, and these veins drain into larger veins that are varied and un-named. From these, the venous blood drains into the larger named veins such as the temporal or facial vein, and from there to the jugular vein, superior vena cava and right heart. Therefore, when assessing a vein that looks like a branching tree, remember that the blood flow is from peripheral to central and it is actually a collection of tributaries draining to a central vein.
As the most superficial veins will join together and drain into slightly deeper veins, and these deeper veins might do the same again, one sort of problem vein might be associated with another sort of problem vein of different size and depth. Hence no classification of problem vein to be treated can be rigidly defined. Problem veins that need treatment might cross between two or more types of facial veins.

Figure 1: Telangiectasia (thread veins) on the chin as distinct veins in a group.
Suitable for treatment with advanced electrolysis/radiofrequency (electrocautery) or transdermal laser.

Figure 2: Diffuse redness of cheek suitable for treatment with IPL.
Telangiectasia (‘spider’ or ‘thread’ veins)
Telangiectasia are classically very fine veins that are very superficial (Figures 1 and 2). If bright red, the blood is usually in small arteries that lie before the capillaries, whereas if the blood is blue or purple, it usually lies in veins after the capillary network [1]. The veins themselves are colourless, appearing white when empty. The colour of veins only comes from the blood within the vein. The thicker the vein wall and the deeper the vein, the more the colour changes from blue through to green until eventually, when the vein is deep enough, there is no colour seen in the veins which are sub-dermal.
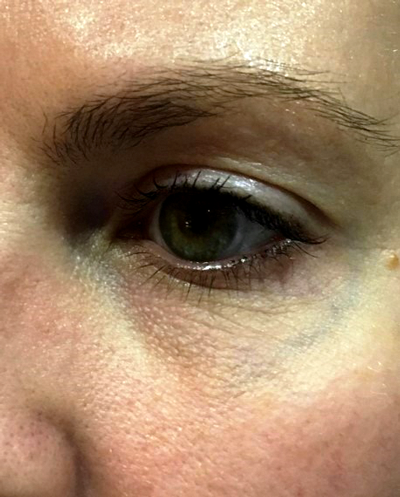
Figure 3: Periorbital reticular vein. Green in colour and not raised, so suitable for
treatment with transdermal laser – usually ND:YAG (1064nm) for this sort of vein.
Reticular veins
Reticular veins are veins that are seen as a green line through the skin, but without any bulging (Figure 3). This is the same name as given to reticular veins in the legs or elsewhere in the body. The fact that they appear to have a green colour is very important when it comes to possible treatments.
Subdermal veins
When veins are both big enough and deep enough, they can make the skin bulge above them, giving the appearance of a ‘varicose vein’. Of course a ‘varicose vein’ of the face is not really a varicose vein as we would understand it in the legs. In the legs, such varicose veins occur because the valves fail and blood accumulates in the vein due to gravity. In veins in the face, blood falls with gravity back towards the heart. However, these veins can still dilate, causing cosmetically unsightly bulges, particularly when certain provoking manoeuvres are performed such as smiling, talking, straining or leaning forwards. A new sign, never described to our knowledge before this article, is the ‘Whiteley-Smith provocation sign’ for forehead veins. In this new sign, subdermal veins of the forehead appeared after manual compression of the cheeks (Figure 4). This mimics the dilation of the same veins seen with the other provoking manoeuvres identified above. These veins tend to show no colour as they are deep to the dermis and the colour of the blood cannot be seen through such a thick layer of vein wall and skin.

Figure 4: The Whiteley-Smith provocation test for forehead veins. Patients often say that forehead veins are only visible when they smile, laugh, exercise or are hot. This simple sign, pressing on the cheeks beside the nose, occluds the facial vein and shows the forehead veins in the dilated state even when sitting upright.
As any practitioner will know, and as pointed out at the beginning of this section, there is quite a crossover between reticular veins and subdermal veins. Quite often green reticular veins will start bulging as they get larger and deeper. Similarly, telangiectasia can often be seen to be draining into a green reticular vein. Therefore, when it comes to assessment and treatments, careful notes should be taken as to the target vein that the patient wants treated and sometimes more than one treatment strategy is required to get rid of the whole complex of problem veins.
Basic classification of facial veins – anatomical position target veins
As noted before, there are certain areas of the face that are associated with certain sorts of veins that patients want to have removed.
Cheeks, chin and nose
Most patients presenting with ‘facial veins’ present with veins in these areas and so aesthetic practitioners will be most comfortable with these patients. The veins in these areas tend to be telangiectasia. They are usually bright red (often being arterial even though they are still referred to as veins), but can be darker, tending towards purple or blue. When darker, they tend to be larger and slightly deeper. They can occur individually, in small groups (Figure 1), or can occur in large patches (Figure 2). On the cheekbones, such red patches showing a large number of thread veins can indicate sun-damage. This is different from a ‘diffuse redness’ commonly known with the public as having a ‘high colour’ or ‘skin flushing’. This is a generalised redness of the skin rather than individual telangiectasia. Such ‘high colour’ can be clinically referred to as rosacea.
Many patients present with complaints about telangiectasia around the nose. These can be individual or in small groups. They often occur around the nasal alar (the skin crease between side of lower nose and cheek) or at the entrance to the nostril, or can be on the nose itself. When there are a large number of telangiectasia on the bulb of the nose, the nose can look particularly red. This is often thought to be associated with heavy alcohol consumption and many people get very embarrassed by it. Of course, alcohol may be the cause in some patients, but in a great number of patients it is not. Also, be careful of conditions such as rhinophyma when the soft tissue of the nose is enlarged and the skin red. If the contours of the nose are abnormal, do not think the problem is merely telangiectasia and be sure to get an expert ENT opinion before thinking of treatment options.
Periorbital areas
Many patients complain of reticular or bulging veins in the periorbital areas. These are usually directly under the eye or under and lateral to the eye (Figure 3). They can be blue / green and not raised or can be bulging. Often they are both. When present, they can appear in isolation, or can be bilateral. Commonly, they are also associated with veins in the temple area and can often be seen to be continuations of the same veins (Figure 5).

Figure 5: A combination vein complex with a bulging sub-dermal periorbital vein
(marked with surgical marker) which is suitable for phlebectomy
and temporal veins suitable for transdermal laser (ND:YAG).
Temples
Increasing numbers of patients are coming to see us with veins in the temple area. These appear to be a branching tree arising from a single vein at the lateral side of the eye, and a fan of several veins branching up towards the hairline. Of course in reality, they are tributaries coming from the hairline and coalescing into a single vein at the lateral corner of the eye, as the blood is draining from the scalp into this vein. It is useful when thinking about treatment, to think of the vein as a ‘tree’ branching up from the lateral eye, but when thinking of the problems with sclerotherapy, it is well worth remembering that the blood is flowing down these veins towards the orbit.
These veins drain into the main facial vein, but also can drain into veins inside the orbit and around the eyeball, and from there into the sagittal sinus. This is one of the major venous sinuses between the cerebral hemispheres of the brain. A sagittal sinus thrombosis, although rare, is a disaster and should always be at the back of your mind when treating veins in this area.
The veins that are near the hairline are usually green / blue and rarely bulge too much. However, the vein at the lateral part of the eye that they drain into is often bulging and is sometimes too deep to show colour. This vein can often be linked to a periorbital vein running from beneath the eye.
Forehead
Problem veins of the forehead are almost always large, fairly vertical, cause considerable bulging and rarely have colour. They run beneath the dermis and so usually, no colour is visible through the skin. They are large, and hence cause the bulging of the skin above them. Sometimes they can be single, running from hairline to a place between the eyebrows. Sometimes they can be multiple. Patients often say that these veins make them look like a ‘Klingon’ (a reference to the TV series Star Trek), and that they tend to ruin holiday photographs, being prominent in the heat and when patients are smiling, causing shadows on the forehead in photographs.
Treatment options
The most important principle to remember is that facial veins lie above the heart. As such, we do not have to consider gravity, failure of valves or venous reflux when assessing and treating facial veins. Conversely, telangiectasia or varicose veins of the legs are situated below the heart and are therefore almost always associated with gravity problems. These veins usually are associated with the failure of valves in the underlying veins of the legs or pelvis, and venous reflux with gravity.
Therefore, the whole approach and understanding of facial veins is completely different from that of veins of the legs, as are the treatments. If you are using the same approach and treatments as you would for leg veins, then you are mistreating one or other of these groups of patients.
Fortunately, for aesthetic practitioners dealing with facial veins, these are easier to assess and treat than leg veins. Unlike leg veins, we do not need to get venous duplex ultrasonography to look for underlying valve failure in these veins. Treatment options for facial veins can almost always be selected from visual assessment alone.
When thinking about possible treatment options, the selection of the appropriate treatment comes down to colour, size and depth of the target vein with a small consideration as to the location once the other factors have been taken into account.
Unlike the skin of the leg, the skin of the face is constantly exposed to ultraviolet radiation from the sun and is therefore very resistant to thermal damage. As such, transdermal laser can be used directly to treat appropriate facial veins with low chances of causing skin burns. This is the reverse of what is found in treating leg veins. The skin on the legs is rarely exposed to ultraviolet radiation and as many aesthetic practitioners have learnt to their cost, trying to perform laser on leg thread veins often leads to skin burns. These burns do not become apparent until three months after the treatment due to the healing process of the skin after a burn.
Advanced electrolysis / radiofrequency ablation (electrocautery)
One of simplest ways to treat individual veins is to use heat generated at or near the point of a needle. Electrolysis machines and radiofrequency machines, although often marketed as different technologies, have the same basic characteristics and indeed use the same needles. An alternating current is passed into the needle (‘monopolar’), making the tip positive, followed by negative, followed by positive and so on, rapidly changing the current and hence polarity. The rate at which the current alternates (and hence the polarity of the needle) ranges from thousands of times per second (kilohertz or KHz) to millions of times per second (megahertz or MHz). This alternating polarity attracts electrons in the tissue then repels them at these very high frequencies, generating heat in the tissue. Alternatively, a two electrode approach (‘bipolar’) can be used with two needles or other conductors with an alternating current between them at the same high frequencies.
When the tip of the monopolar needle is placed on a very superficial vein, heat is generated in the tissue destroying epidermis and vein, and if deep enough sometimes superficial dermis. Although electrolysis is often dismissed as a treatment to remove hair only, advanced electrolysis techniques such as red vein removal can be highly effective in experienced hands. Increasing the alternating current from kilohertz to megahertz and calling the procedure radiofrequency ablation is very good marketing, but there is little scientific evidence that the results are different using the different frequencies found in electrolysis machines or radiofrequency machines.
Electrocautery devices are relatively cheap and as the techniques are effective [2] and suitable for individual or small clusters of veins, they should be part of any practice treating facial veins.
Sclerotherapy
The use of sclerotherapy in facial veins is controversial. Sclerotherapy is used to treat small veins on the legs and body and when made into a foam, has been used to treat larger veins. A quick search on the internet will show that many practitioners offer sclerotherapy for facial veins. However, experts in the field have pointed out that sclerotherapy “can be used on larger blue telangiectasia but may be complicated from inadvertent injection into arterioles” [1]. This can lead to skin necrosis or, very rarely, blindness in one eye [3].
Furthermore, sodium tetradecyl sulphate (STS), the most commonly used detergent sclerosant in the UK, is not licensed for use in facial veins, and the nursing and midwifery council (NMC) has already ruled in one case where STS was used and a complication ensued [4]. In the UK, practitioners can use products for unlicensed indications, but should be able to explain that no licensed medication or technique would be able to be used instead. As there are other techniques to treat all sorts of facial veins, which do not involve the risks of sclerotherapy, it is hard to see how practitioners can justify using sclerotherapy for facial veins. Although complications are rare, when they do occur they can be severe [5]. As such, we do not recommend the use of sclerosants for any facial veins despite some authors having published good results in their own hands [6].
Intense pulsed light (IPL)
IPL machines produce very concentrated and well-controlled bursts of white light in pulses. This white light also includes some infrared and ultraviolet wavelengths, ranging from about 400nm through to 1200nm [7]. A variable number of pulses can be chosen, each of the defined length, with a defined length of rest in between each pulse. The white light is at an intensity that it will heat tissue. Different hand pieces then put different filters in the way of the white light before it hits the skin. For red vein treatments, a yellow filter is used. This filter allows a relatively narrow band of wavelengths of light through it, around 500nm wavelength (yellow light). As the absorption peaks for oxyhaemoglobin (predominantly found in red veins) and deoxygenated haemoglobin (predominantly found in blue veins) are 418nm and 542nm respectively, this is ideal for facial telangiectasia. IPL handpieces often have a wide ‘footprint’ meaning that quite large areas can be treated with each shot fired. Thus, IPL is ideal for large areas such as for diffuse telangiectasia or rosacea.
Transdermal laser
LASER is an acronym for light amplification by the stimulated emission of radiation. Although some lasers do produce light, others produce microwaves which are invisible to the naked eye. Originally these used to be called MASERs but now tend to be called LASER as well for simplicity. Unlike IPL, which uses white light and then selects bands of wavelengths using filters, laser produces light of one wavelength only. This is called ‘monochromatic’ light. In addition, all of the photons (individual rays of light) in a laser are precisely aligned or ‘in step’. This is called coherent light. When light photons are all lined up ‘in step’ with each other, they can carry a tremendous amount of energy.
As a laser produces a precise wavelength, the appropriate laser can be chosen to target any particular pigment such as oxyhaemoglobin or haemoglobin. When such a pigment or chemical is targeted by laser, it is called a ‘chromophore’. Chromophores absorb or reflect different wavelengths of light. When it absorbs sufficient energy, it can be disrupted or can heat up. Therefore, for vascular lesions such as thread veins on the face, a wavelength is used that is readily absorbed by oxyhaemoglobin or deoxygenated haemoglobin. Such lasers include the KTP (532nm – green light) and the ND:YAG (1064nm – microwave) lasers although other lasers can also be used. The KTP does not penetrate very deeply and so is used for very superficial veins that are bright red or bright blue. It heats the haemoglobin, causing the heat to be passed into the vein wall and destroying the vein. The ND:YAG, which has a wavelength exactly twice that of the KTP, also interacts with haemoglobin causing it to heat. However, this longer wavelength penetrates deeper into the skin, allowing larger green veins to be treated that lie deeper under the skin. It is effective to at least 1.5mm deep to the skin.
Lasers allow many different factors to be changed. The area to be treated for the ‘spot size’ can be varied, allowing for individual veins to be targeted with a very small spot size or areas with a larger spot size. Different powers can be used and when a power is selected, this is divided by the area of the spot, giving the ‘fluence’ (power per square centimetre of skin). In addition, the pulse length can be varied. Pulses are usually in the range of milliseconds. This variability makes laser a very flexible tool to use, although it needs considerable experience to master. Many aesthetic companies pre-programme settings for different lesions, allowing those who are not very experienced to have a relatively safe, if not individualised, treatment setting.
Therefore, with access to lasers of different wavelengths and different spot sizes and powers, telangiectasia and reticular veins can be treated in the majority of cases. As a general rule, if the vein has colour and is not large and bulging, then laser can usually be used if the correct wavelength and settings are selected. Furthermore, as the skin of the face is always exposed to sunlight, it is quite resistant to burning. Therefore, it is quite resistant to high laser powers, allowing high energies to be passed into veins to be treated without damaging the skin. This is the reverse of the situation in the legs where the skin is sensitive to burning and transdermal laser for leg thread veins frequently ends up in permanent burns leaving white scars.
Phlebectomy
Phlebectomy of facial veins is technically difficult and requires considerable practice. In our experience we find it useful for larger bulging veins particularly in the periorbital, temporal and forehead regions. In particular, veins in the centre of the forehead are often very large, subdermal, and therefore show no colour. These are too deep and large for electrocautery, IPL or transdermal laser and with the high flow rates potentially flowing through them into the orbital veins, sclerotherapy is not a sensible option [3].

Figure 6: Forehead veins, bulging and too deep to see any colour. Suitable for phlebectomy under local anaesthetic, a far more complicated procedure than phlebectomy elsewhere on the body due to the muscles of facial expression inserting into the skin.
We prefer phlebectomy using local anaesthetic (lignocaine) with adrenaline (epinephrine) to reduce bruising. Incisions are made using the smallest possible blade and in line with where skin creases will develop if there are none present. Of course if there are skin creases already, incisions should be made within these. Phlebectomy hooks can be used but it should be noted that these veins are very small and difficult to remove. They are often adhered to the skin and access with the hook is difficult due to the muscles of facial expression (frontalis muscle on forehead) inserting into the skin around the vein. With experience, good results can be obtained (Figure 6) but we have found it is a long learning curve to get good at this and so we restrict the practice to one surgeon in our clinic. In addition, we have ready access to vascular ultrasound which is helpful in identifying the position of veins, checking there is no arterial flow and ensuring that there is no abnormality associated with the target vein (Figure 7).
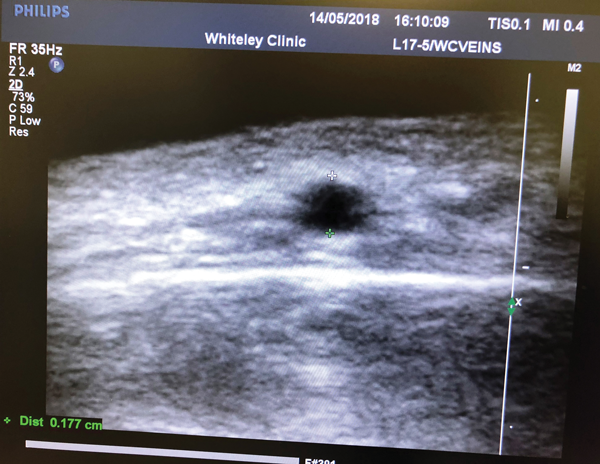
Figure 7: Ultrasound of forehead vein in transverse section.
The scale shows that the vein is 0.177 cm in diameter and is about the same depth.
Wounds are easily closed with Steri-Strips and patients are warned that bruising can take up to four weeks to disappear, and the wounds similarly up to four weeks to disappear. Patients are advised not to go out in the sunlight during the healing process. Apart from scars and bruising, patients must be warned about the risks of infection, failure to remove the vein completely, poor cosmetic result and damage to surrounding tissues including sensory nerves. We have recently had a case where a patient had previously undergone surgery to his brow, with an incision across the top of his head above the hairline and the skin and muscle reflected down off of the frontal bone. At subsequent surgery the veins were so scarred that they could not be removed surgically. Hence previous surgery in the area of facial veins is now a contraindication to phlebectomy in our unit.
Facial phlebectomy is not something to be performed by anyone who has not got a very good understanding of the anatomy of the area, who has had some training by an experienced trainer and who is performing the procedure regularly enough to ensure they get through the learning curve and maintain their experience.
Conclusion
The treatment of facial veins is a common aesthetic procedure. As a general rule, the smaller and more superficial the vein, the easier they are to treat and the more commonly they are treated. A good understanding of the different veins that can be encountered and the different methods of treatment that are available, will enable an aesthetic practitioner to know which veins they are comfortable treating with a high chance of a good result, and which veins they should refer to practitioners that specialise in the more difficult and less common facial veins.
Finally, as with most (if not all) aesthetic conditions, there is no medical need to treat every facial vein merely because the patient requests it. Practitioners should keep a high index of suspicion as to any lesion that might be presented as a ‘facial vein’ but doesn’t look typical, and should not feel obliged to treat every patient who attends for consultation. Atypical vascular lesions should be referred to appropriate specialists for a second opinion.
References
1. Goldman M. Optimal management of facial telangiectasia. Am J Clin Dermatol 2004;5(6):423-34.
2. Liapakis IE, Englander M, Sinani R, Paschalis EI. Management of facial telangiectasias with hand cautery. World J Plast Surg 2015;4(2):127-33.
3. Arunakirinathan M, Walker RJ, Hassan N, et al. Blind-sided by cosmetic vein sclerotherapy: a case of ophthalmic arterial occlusion. Retin Cases Brief Rep 2017; [Epub ahead of print].
4. Bartlett N. Liverpool nurse warned after falsely claiming to have celebrity client and gave botox to patient without proper prescription. Echo 2014.
www.liverpoolecho.co.uk/news/
liverpool-news/liverpool-nurse
-warned-after-falsely-7309680
Last accessed October 2018.
5. Roberts E. Lisa Fairbanks left with lasting ill-effects after treatment to remove a blemish went badly wrong. Basingstoke Gazette 2014.
www.basingstokegazette.co.uk/
news/11660759.Blemish_removal
_ends_in_agony_for_Basingstoke_mum/
Last accessed October 2018.
6. Green D. Removal of periocular veins by sclerotherapy. Ophthalmology 2001;108(3):442-8.
7. Goldberg DJ. Current trends in intense pulsed light. J Clin Aesthet Dermatol 2012;5(6):45-53.
Declaration of competing interests: None declared.
COMMENTS ARE WELCOME




