Rhinophyma is an aesthetic embarrassment to many people. It is the result of sebaceous gland hyperplasia within the skin over the alar cartilages of the nose. It has a familial tendency and in addition to being unsightly it can commonly cause problems with infection and pustular greasy secretions.
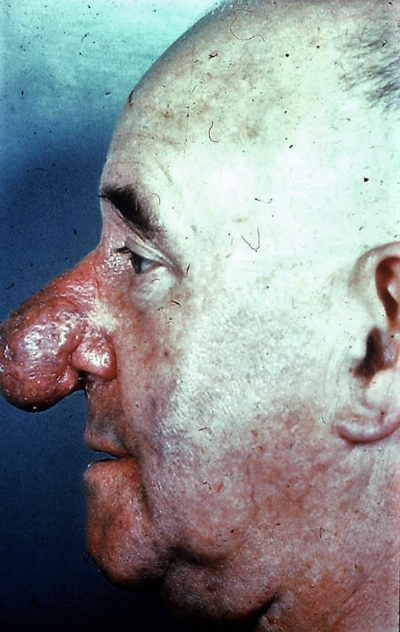
There is a range of clinical severity from the most minor, where the skin surface is relatively flat but enlarged pores are evident and readily produce sebaceous material when squeezed, and topical non-invasive skin treatments and antibiotics can control infective pustular episodes, to the most major where there is significant thickening and nodularity causing additional misshape to the tip (Figure 1). The latter is extremely depressing for the patient. In clinical practice many affected individuals refer for rhinoplasty not realising that skin thickness is one of the most important considerations in determining satisfactory outcome from rhinoplasty, especially in men and it may be actually the skin itself not the underlying cartilages that require attention [1].
Figure 1: Severe pustular and nodular rhinophyma.
General principles
In mild cases of rhinophyma improvement can be sought using surface ablation techniques that include the superficial to deep dermis (Figures 2a & b). The superficial epithelium is obviously destroyed but not where it penetrates into deep fissures and crypts or in deeply sited adnexal structures. Success lies with avoidance of postoperative infective episodes, improvement in appearance and improved psychological affect in the patient. The more superficial the injury the faster to heal and less likely that hypopigmentation or hypertrophic scar will develop.


Figure 2a & b: Pre and one-year post treatment
of mild rhinophyma using superficial plasma.
Thick sebaceous rhinophyma needs a more aggressive approach to cause a deeper dermal ablation (Figures 3a & b) and in severe cases there is no other option other than to excise or surgically shave the offending tissues down to the perichondrium. The results are quite acceptable (Figures 4a-c and Figures 5a & b).



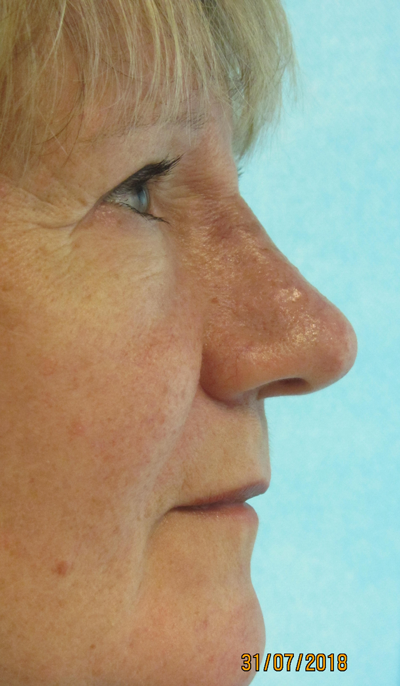
Figure 3a-d: Pre and post treatment of thicker rhinophyma using a more penetrating depth of plasma via multiple passes in a pair of identical twins. Even at an early stage (six weeks) both patients are highly delighted. The wounds were fully healed within 10 days.


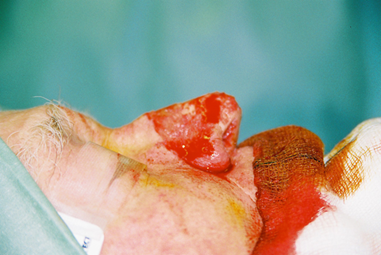
Figure 4a-c: Shaving the nodular sebaceous tissues causing severe pustular rhinophyma in a 65-year-old man. The thick tissue is shaved almost to the perichondrium using a number 10 Swan Morton surgical blade.
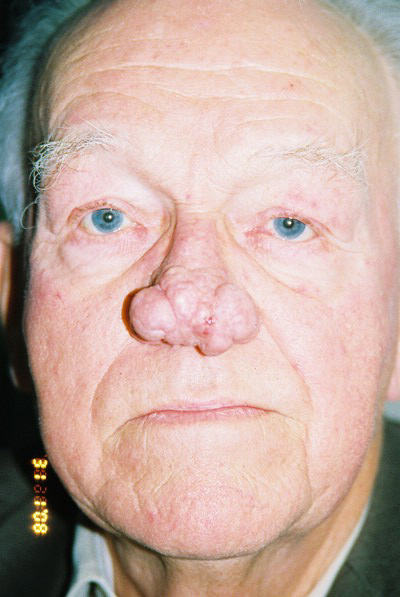

Figure 5a & b: Pre and postoperative frontal view six weeks later of the same patient with severe pustular and nodular rhinophyma shown in Figure 4a. Depigmentation and fragile skin are apparent at this stage but the contour has significantly improved.
In between is the moderate to deep pore rhinophyma and this is best treated as conservatively as possible in the first instance but a skin ablation at least into the mid-dermis of the rhinophyma is required. Success is therefore achieved by controlling the depth of skin injury required to smooth contour irregularities but also to avoid variable pigmentation, hypertrophic scar disfigurement and secondary sepsis from blockage to sebaceous gland secretion. Biofilm probably plays a part within hypertrophic scar development, so wound contamination should be minimised.
To create such an intradermal injury, dermabrasion was commonly practised before the 1980’s and ablative lasers were introduced thereafter. Coarse diamond burrs were used for dermabrasion and were quite effective but there was risk related to a significant amount of hazardous, infected or potentially contaminated microdroplets released by an aerosol effect into the theatre environment. Laser therapy is ablative but repeat passage is required and there is a limit to controlling the depth of injury. The dot matrix pattern created by laser does not offer a constant flux within the treated area either and circles of hypopigmentation may draw attention to the nose once fully healed.
An alternative method to reduce risk in treating moderately deep rhinophyma is by utilising thermal energy from a plasma source. The Nebulaskin Plasma delivery system (Fourth State Medicine, Surrey, UK) is a non-pulsatile, continuous flow thermal energy source used with a paintbrush technique to provide a controlled depth of burn injury.
Use of plasma for superficial and deeper dermal ablation
Plasma has now been used successfully to treat three patients with moderate and distressing rhinophyma (Figures 2a & b and 3a & b). Investigations on the depth of dermal injury created by plasma had been studied previously [2]. Under general anaesthetic the rhinophyma skin was prepared using aqueous chlorhexidine and treated with as many passes of continuous focused plasma energy as was necessary to cause a mid-dermal injury. In these cases two passes were adequate. It would have been perfectly reasonable to treat these rhinophyma cases under local anaesthetic if the rhinophyma had been in isolation, but these patients were having combined surgical procedures. The sloughy resultant superficial eschar was wiped using a dry swab with lateral friction to reveal a fixed stain, red base indicating a clean intradermal injury (Figure 6).



Figure 6a-c: Perioperative view of deep dermal nasal skin injury in one of the twins shown in Figure 3 after the slough has been wiped off from the surface of plasma treated rhinophyma. Note the fixed red stain. This is not a full thickness skin injury and healing occurs within 10 days. A deeper dermal injury becomes a paler colour. Two lentigo simplex lesions on the right cheek were more superficially treated with one pass of plasma and the superficial epidermis was wiped off using a dry swab. The result at six weeks shows significant improvement in skin texture with no apparent depigmentation or evidence of hypertrophic scar.
The process can be repeated depending upon the required depth of treatment but the subsequent intradermal injury obviously cannot be wiped away. In moderate rhinophyma ablation to deepest dermis is not actually required and may create risk of poor scar and de-pigmentation. The aftercare advice was simply to keep the area clean from debris using a propriety brand antiseptic soap such as Carex (Cussons, UK). No patient complained of pain in the recovery period and no regular analgesics were required.
The nose is quite remarkable for its ability to heal rapidly and leave good quality, but thinner, dermal skin with a protective and stable epidermis. The plasma injured site behaves like any acute burn wound and once healed there is a transient phase of inflammatory redness that settles within a few months. In the interim, cosmetic camouflage is very effective in improving the appearance of the maturing wound. Skin protection to UV light is important thereafter and the skin must be kept moisturised.


Figure 7a & b: Pre and postoperative view of a series of basal cell papillomas, easily wiped off the skin in a clean cleavage plane at the dermal-epidermal junction after superficial single pass ‘paintbrush’ treatment with Nebulaskin. There is a very superficial dermal injury and healing occurs within one week.
The latest version of Nebulaskin has a three-way setting for the new ‘slimjim’ hand piece to provide different levels of dermal injury. For superficial epidermal type lesions the low power setting easily removes epidermis and is ideal in treating basal cell papillomas (Figures 7a & b), for the deepest dermal ablations, such as required in rhinophyma. The highest power setting speeds up the process and avoids repeated passages. The middle setting on the ‘slimjim’ will work well on perioral wrinkles.
References
1. Frame JD, Bagheri SC, Smith DJ, Khan HA. Aesthetic Surgery Techniques – A Case Based Approach. Elsevier: 2018;111-66.
2. Kamel D, Frame JD, Harle T. Histological Findings from Controlled Application of a Thermal Plasma to Human Skin. Clin Surg 2016;1:1176.
Declaration of competing interests:
Professor Frame financially contributed to a research fund at the University of Surrey Space Centre to help initiate lab-based research for a terrestrial use of plasma. As such he is a minor shareholder in Fourth State Medicine. Fourth State Medicine is in receipt of multiple research grants investigating applications of plasma in ablative therapy, wound healing, antimicrobial and biofilm therapy. Professor Frame is Medical Advisor to Fourth State Medicine.
COMMENTS ARE WELCOME